Advancing Early Detection of Fetal Anomalies with Detailed First-Trimester Ultrasound
By Brian K. Iriye, MD; Vanita D. Jain, MD; and Anthony C. Sciscione, DO
What is DFTU and Why Is It Important?
The Detailed First-Trimester Ultrasound (DFTU) is a high-resolution scan performed between weeks 12 and 13 of pregnancy to detect fetal structural anomalies.1 It is indicated for pregnancies that have an elevated risk of fetal abnormalities, including maternal obesity, pre-existing diabetes, alcohol and drug use, placenta accreta, abnormal chromosomal and genetic screening findings, and suspected hereditary disease, among other risks.
Detecting fetal anomalies earlier in pregnancy allows for timely counseling, evaluation, and intervention planning for our patients. Discovering fetal problems early is especially important in light of the challenges our patients face accessing abortion care later in pregnancy.
What Can DFTU Detect?
Studies show DFTU identifies approximately 85% of major fetal anomalies and almost one-third of all anomalies by the end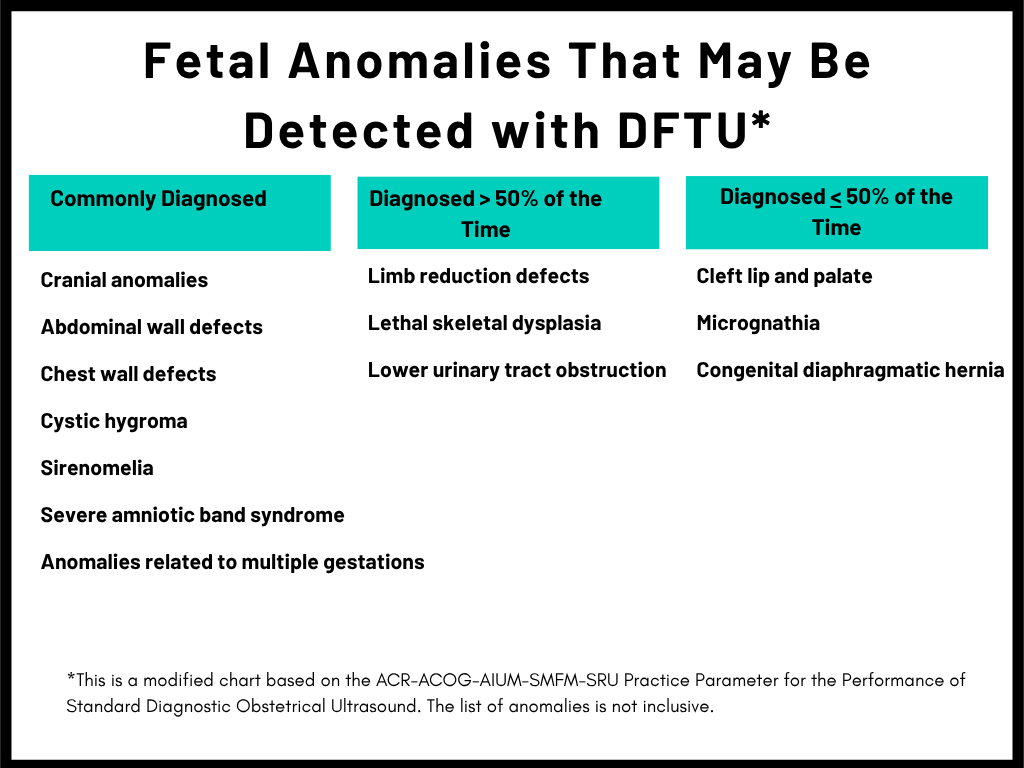 of the first trimester.2 Although not a replacement for detailed second- and third-trimester scans (DSTUs), DFTU offers our patients a critical opportunity to identify serious fetal conditions earlier in pregnancy.
of the first trimester.2 Although not a replacement for detailed second- and third-trimester scans (DSTUs), DFTU offers our patients a critical opportunity to identify serious fetal conditions earlier in pregnancy.
An Evolving Billing Framework
DFTU billing has faced challenges because many payers deny the recommended SMFM combination of CPT® 76801 and CPT® 76813.
Currently, there is no single code to bill for a detailed exam in the first trimester. Since 2018, the Society for Maternal-Fetal Medicine (SMFM) has been working with the American College of Obstetricians and Gynecologists (ACOG) and other medical societies to determine the best method for DFTU billing. SMFM advocated for a temporary solution that combined the 76801 (fetal anatomy first trimester) code with the 76813 (nuchal translucency (NT)) code.
As prenatal diagnosis has evolved and our organizations more strongly support the use of non-invasive prenatal testing, the use of the NT scan alone has fallen out of practice. After the 2023 closure of the US Perinatal Quality Foundation, the credentialing body for the Nuchal Translucency Quality Review program, ACOG, American College of Osteopathic Obstetricians and Gynecologists, American College of Radiology, American Institute of Ultrasound in Medicine (AIUM), SMFM, Society of Diagnostic Medical Sonography, Society of Family Planning, and the Society of Radiologists in Ultrasound, worked to develop a solution to these challenges. Based on expert advice and discussions with the American Medical Association and other stakeholders, it was determined that utilizing an existing code would be the best approach. In looking at the characteristics of DFTU, it most closely aligns with the same images obtained on a second-trimester detailed ultrasound – CPT® code 76811.
CPT 76811 was never restricted to a single use per pregnancy. The adoption of CPT 76811 for DFTU addresses payer denials and aligns payment with the increased time, skill, education, and resources required for clinicians. This guidance:
- Clarifies that CPT 76811 can be billed once before and once after 14 weeks of gestation, per pregnancy and facility.
- Aligns with the AIUM practice parameter for detailed anatomic ultrasound exams during the first trimester.
- Encourages high-quality practice by ensuring billing reflects clinical complexity.
It should be noted that transvaginal sonography (CPT® 76817) may be used in conjunction with CPT 76811 when required to achieve optimal imaging in either DFTU or DSTU.
Who Should Perform DFTU?
DFTU is not routine and requires significant clinician expertise. Current guidelines require that providers complete an obstetrics-gynecology residency and a maternal-fetal medicine (MFM) subspecialty fellowship or possess at least one year of ultrasound subspecialty training under the supervision of an experienced provider.
Initial training must include 25 DFTU scans, with five of them showing major fetal anomalies. Ongoing maintenance for providers includes 25 annual scans (five with fetal anomalies) and five hours of relevant continuing medical education every three years. These requirements ensure that DFTU is performed and interpreted by qualified professionals and maintains the highest standards of care.
Marking a Milestone and Moving Forward
The early detection of fetal anomalies in pregnancy is vital as our patients continue to face barriers to comprehensive reproductive options, especially later in pregnancy. DFTU empowers our patients with earlier access to diagnostic information that enables them to make informed decisions about their pregnancies based on their individual circumstances.
The endorsement of CPT® 76811 for DFTU by multiple medical societies marks a key milestone in promoting early fetal anomaly detection, equitable access to care, and appropriate reimbursement. As DFTU’s clinical value continues to grow—particularly in light of increasing limitations on abortion — continued advocacy, training, and access remain essential.
Brian K. Iriye, MD, is past president of SMFM and past president of the Association for Maternal-Fetal Medicine Management. He is currently President of Hera Women’s Health in Las Vegas, NV. Vanita D. Jain, MD, is the former Chair of the SMFM Coding Committee and a past member of the SMFM Board of Directors. Anthony C. Sciscione, DO, also past president of SMFM, is Residency Program Director of Obstetrics & Gynecology at ChristianaCare in Wilmington, DE, and a Professor of Ob/Gyn at Sidney Kimmel Medical College in Philadelphia, PA. Drs. Sciscione and Jain are managing partners at the Delaware Center for Maternal and Fetal Medicine at ChristianaCare.
References
1AIUM. J Ultrasound Med. 2021;40:E1–E16. doi:10.1002/jum.15477
2Lust EER, et al. AJOG. 2025;232(4):396.e1-396.e19. doi:10.1016/j.ajog.2024.07.026
CPT copyright 2023 American Medical Association. All rights reserved.
Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
CPT is a registered trademark of the American Medical Association.
